While healthcare providers would prefer that they not be required to obtain retro authorizations, there will inevitably be circumstances that require the dreaded busy work. However, state Medicaid programs may be slowing down the rate at which services rendered are approved and reimbursed by the program. We have seen an increasing number of retro authorization denials annually across the country, which in many cases result in increased workloads for case management. The work has become so cumbersome that appeal deadlines are often missed, resulting in revenue being left on the table.
In many facilities across the country, case management departments have been charged with ownership of this part of the Medicaid process, which has proven difficult to oversee. An even bigger risk is involved when this work is passed off to the Business Office staff who don’t typically possess the clinical expertise required to be successful in obtaining retro authorizations.
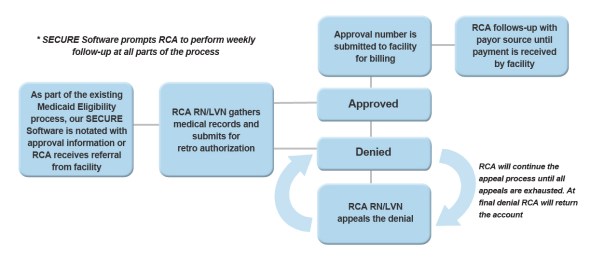
Since RCA provides services as an extension of the hospital’s Patient Financial Services department, we have been asked on several occasions to assist with obtaining retro authorizations after we have successfully secured Medicaid coverage for our patients. The overall process from facility to vendor doesn’t change and the retro authorization and appeal process fits seamlessly into the daily work queues in which we already oversee. Immediately following receipt of the retro Medicaid approval, our expert staff begins the authorization process, shaving off precious A/R days by eliminating any unnecessary hand-offs in the process. In the case of an unfortunate denial, RCA’s clinical staff will make every appeal attempt, and once an authorization number has been approved, it will be submitted to the facility so the account can be billed. Afterwards, RCA will perform routine follow-up to ensure the facility receives payment.
Don’t let retro authorizations and the appeal process put your self-pay reimbursements or A/R days in jeopardy. This piece of the Medicaid process can be easily handled through your facility’s existing eligibility process.

Bethany Bailey
Vice President of Operations and Eligibility Expert
Resource Corporation of America